Dr. Fawaz Al Saryreh lecture
PPt for Dr. Fawaz
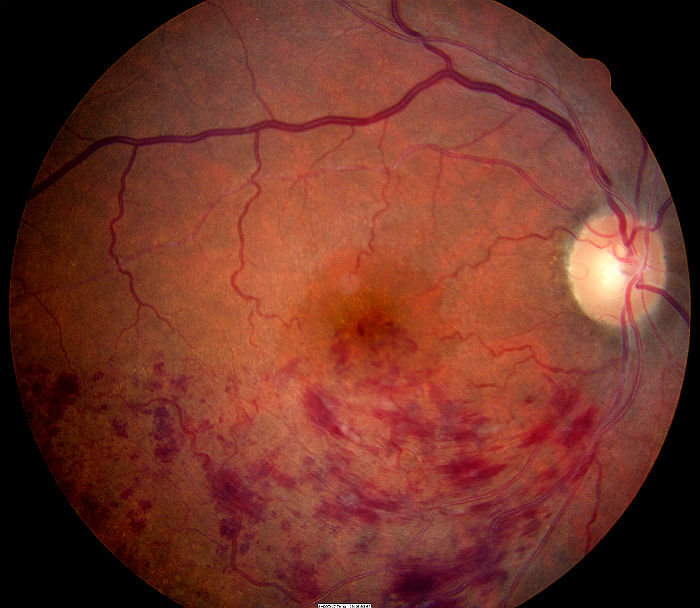
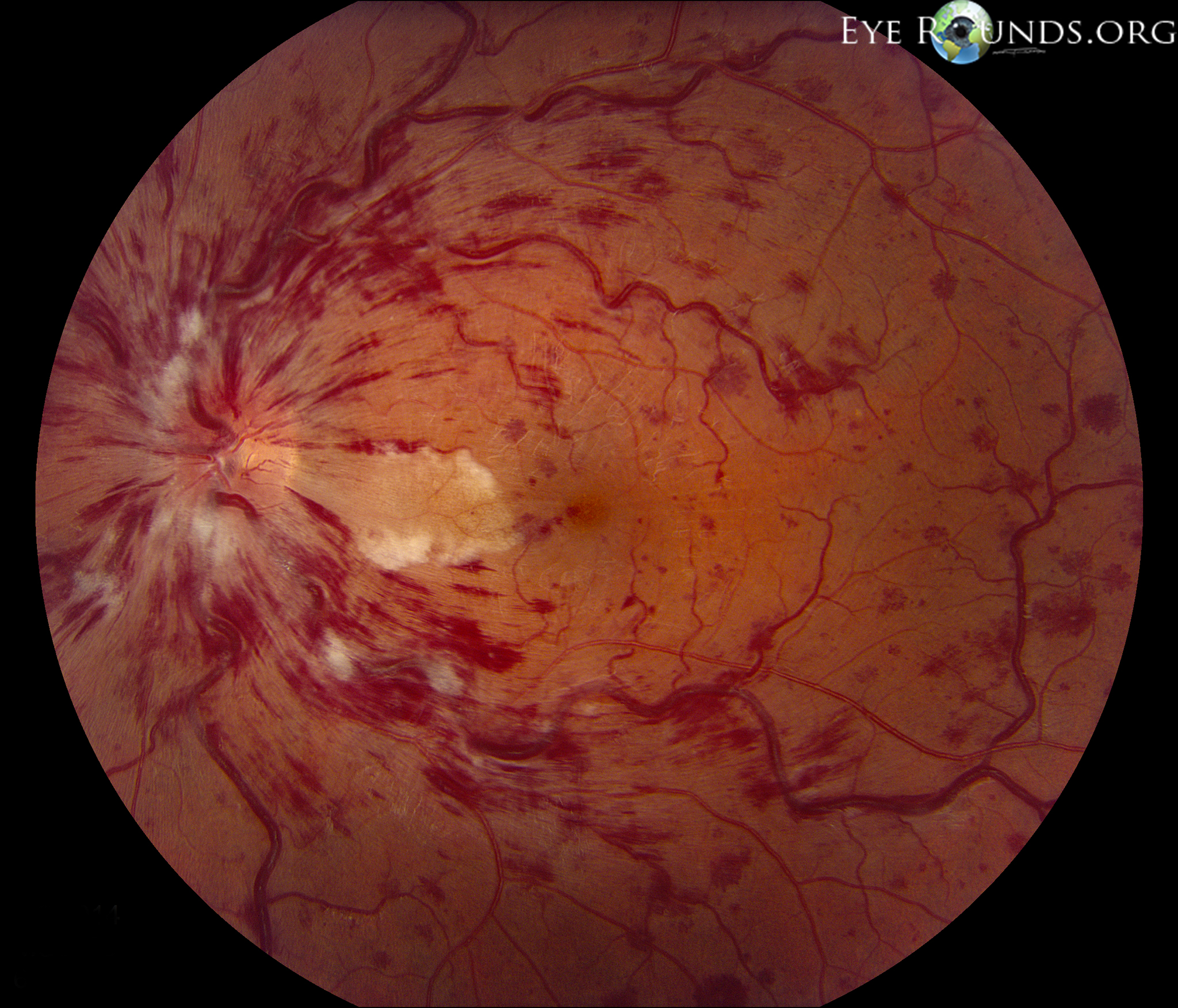
Central retinal vein occlusion:
Central retinal vein occlusion (CRVO) typically occurs in patients over 45 years secondary to retinal vein thrombosis. Risk factors include diabetes, hypertension, hyperlipidaemia, and glaucoma.
CRVO in those aged less than 45 years may suggest a clotting disorder.
Clinical features CRVO produces painless visual loss in one eye. Signs include: retinal haemorrhages in four quadrants; dilated tortuous retinal veins; optic disc swelling; macular oedema; cotton-wool spots; neovascularization of the iris, angle, retina, or disc. Disc collateral vessels are a sign of resolution.
Classification:
■ Nonischaemic.
■ Ischaemic.
1. Clinical examination: RAPD, VA <6/60, multiple cottonwool spots, dense midretinal haemorrhages, ‘blood and thunder fundus’.
2. Fluorescein angiogram: more than 10 disc areas of ischaemia. History and examination Ask about glaucoma, systemic hypertension, raised lipids, diabetes or symptoms of diabetes (polyuria, polydipsia, weight loss).
If younger than 45 years ask about thrombophilia: family history of thromboses aged <45 years; deep vein thrombosis; pulmonary emboli; thromboses in unusual sites, e.g. axillary vein; multiple miscarriages. Examine specifically for new vessels in the angle (undilated gonioscopy), iris, and optic nerve/retina. Examine both eyes for features of glaucoma.
Perform digital ophthalmodynanometry to check for raised central retinal vein pressure. In normal eyes, the central retinal vein spontaneously pulses or can be made to ‘wink’ or collapse with minimal ocular pressure through the eyelids.
In CRVO, the vein and artery ‘wink’ together or, in extreme cases, the artery is more easily compressed than the vein. The latter may also suggest reduced arterial pressure and ocular ischaemia, so compare with the fellow eye, assuming that is normal. Ocular ischaemia may present with loss of VA due to cilioretinal hypoperfusion.
Differential diagnosis Consider ocular ischaemic syndrome; diabetic retinopathy; optic disc swelling for other reasons; and radiation retinopathy.
Investigations Check BP, FBC, ESR, lipids (thyroid function if abnormal), plasma protein electrophoresis, and thrombophilia screen if suspicious. Arrange fl uorescein angiogram if ischaemia is suspected (see Classification above). Diabetic work-up varies from random or fasting glucose, to HbA1c, glucose tolerance test, and diabetologist review. Normal fasting glucose is ≤6.0 mmol; impaired fasting glycaemia 6.1–6.9 mmol; ≥7.0 mmol suggests diabetes, but repeat if there are no diabetic symptoms.

Treatment starts with low-dose aspirin and discontinuation of oral contraceptives. Treat glaucoma (cyclodiode is useful for Arrange panretinal photocoagulation for neovascularization. Consider macular grid laser for patients <50 years with macular oedema and no angiographic evidence of macular ischaemia. Hypertension predisposes to recurrence, so involve the patient’s general practitioner. Alternative therapies Not proven but under review:
■ Laser: chorioretinal anastomosis.
■ Surgical: sheathotomy, radial optic neurotomy.
■ Medical: haemodilution; tissue plasminogen activator; intravitreal steroids.
Follow–up Every 4 weeks for the first 3 months, then as clinically indicated. The Royal College of Ophthalmologists recommend follow-up for 2 years.
to down load UK guidlines on who to treat CRVO, click the following link.
Retinal-Vein-Occlusion-RVO-Guidelines-July-2015
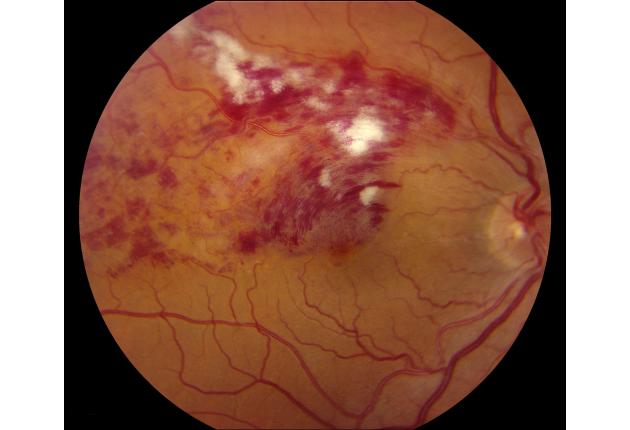
Branch Retinal Vein Occlusion
Background Branch retinal vein occlusion (BRVO) occurs 2–3 times more commonly than central retinal vein occlusion (CRVO) but has similar risk factors.
The main sequelae are macular oedema and vitreous haemorrhage from disc, and retinal new vessels. BRVO affecting the entire superior or inferior retina (hemicentral vein occlusion) has a higher risk of rubeosis and disc new vessels.
Symptoms Usually painless loss of vision in one eye but may be asymptomatic.
Rubeosis is less common; macular oedema, disc and retinal new vessels, more so.
Classification
■ Ischaemic: >5 disc areas of ischaemia on fluorescein angiography.
■ Nonischaemic: <5 disc areas on angiography.
1. With macular oedema.
2. With macular ischaemia.
History and examination Similar to CRVO. Fully exclude systemic causes in patients with multiple BRVOs.
Investigations Same as for CRVO.
Treatment Arrange macular laser at 3 months if there is no macular ischaemia and VA remains <6/12 from oedema. Treat neovasculization with scatter retinal laser.
Follow–up The Royal College of Ophthalmologists’ recommend 3 monthly review for up to 2 years.
Nonischaemic or treated BRVO may require less frequent review.